A soap note template is a structural format used by medical professionals to record the health of patients and their present condition. It can be more or less serve as a prescription. This document acts as evidence that patient is being treated regularly and effectively by different health workers.
Table of Contents
What are SOAP notes?
In the 1960s, a brilliant doctor named Lawrence Weed was created and developed a soap note. During those times, objective documentation didn’t exist. With the help of SOAP notes, the main physician can identify each note that was made and connected with a concern. Moreover, these notes provided health professionals a great way to communicate with each other by using a structured and organized format. These notes have made communication and documentation a lot easier.
Above all, soap notes generate an organized and standard method for documenting any patient data. It makes the health provider able to gather information about a patient from different sources. It also makes sure that the treatment procedures are accurate.
Elements of SOAP notes:
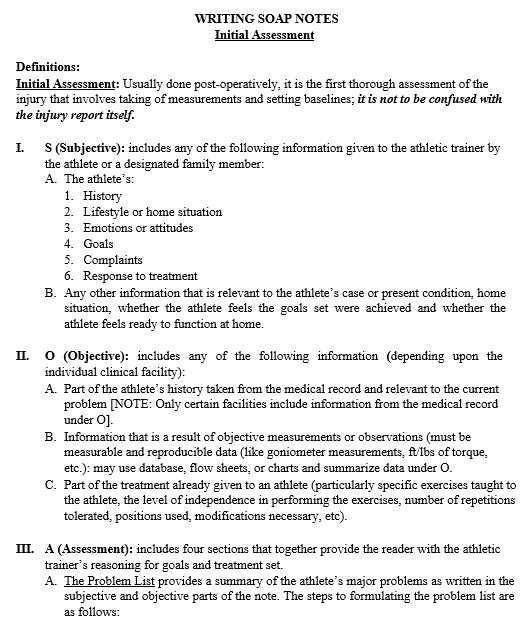
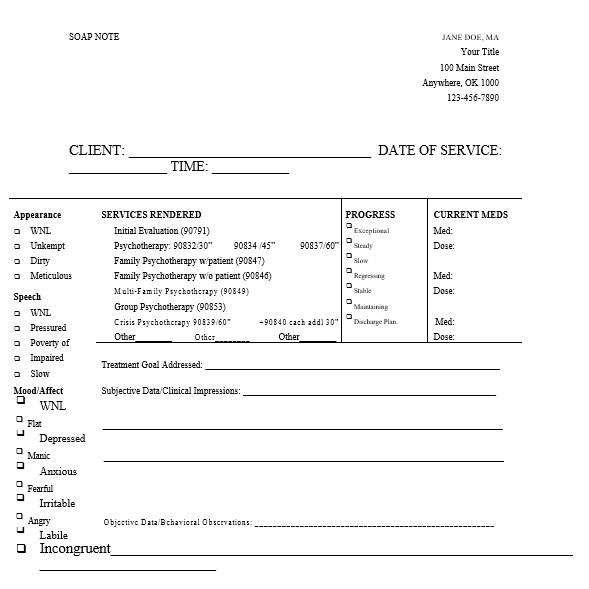
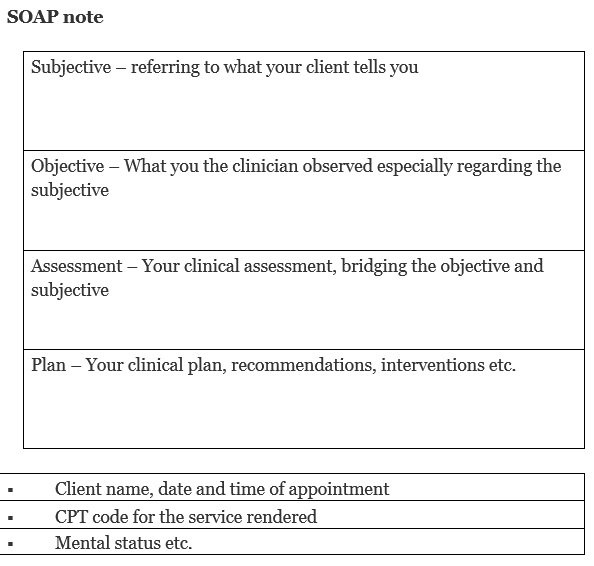
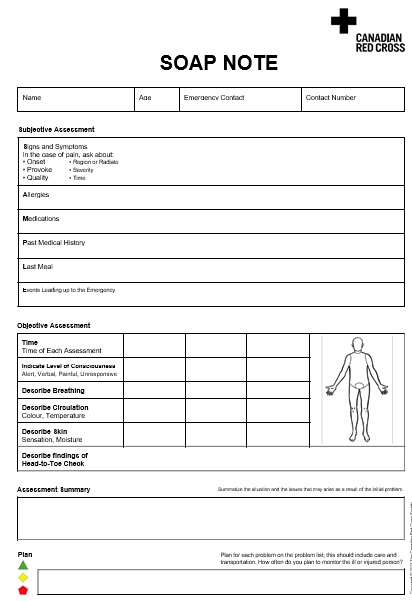
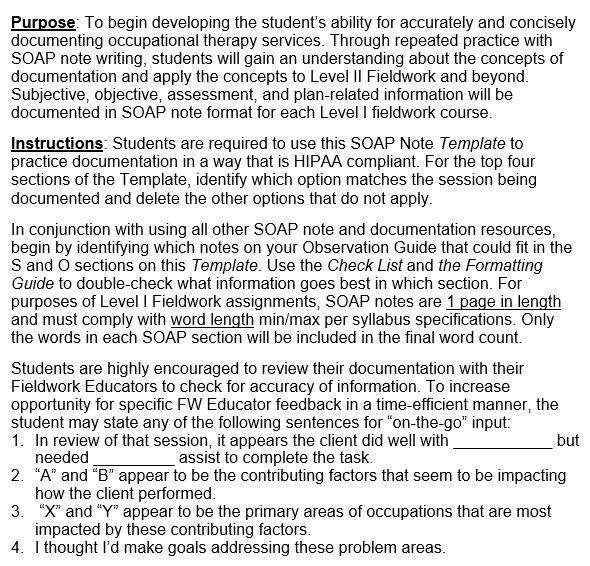
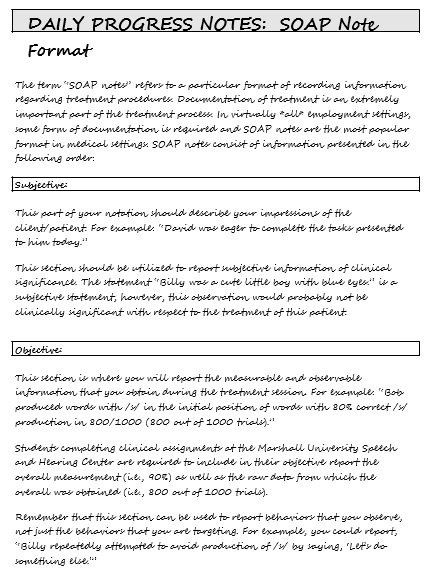
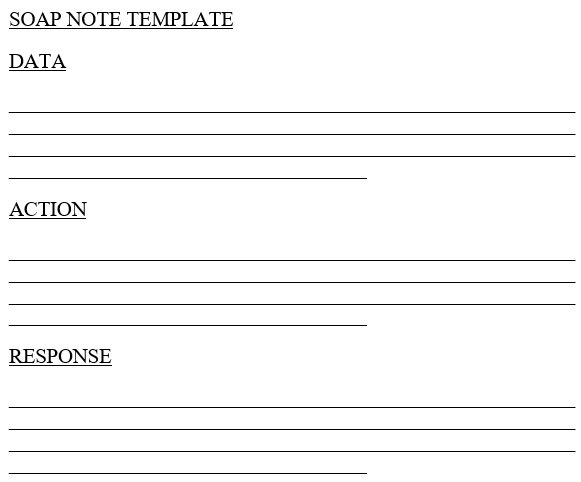
SOAP is actually an acronym and it refers to different components such as subjective, objective, assessment, and plan. Let us discuss these components in detail;
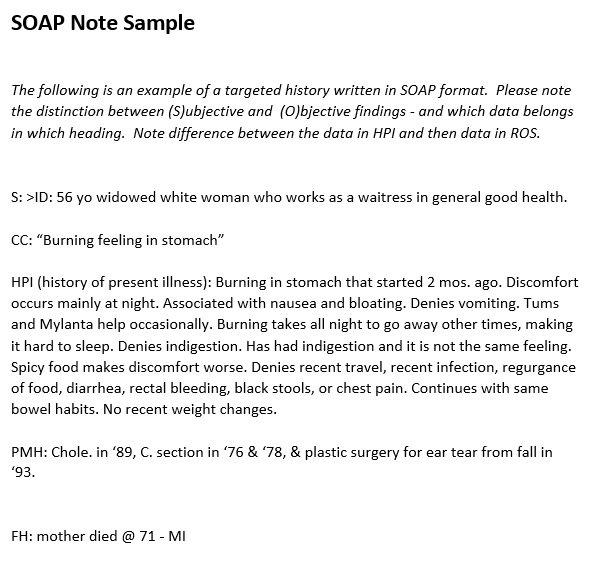
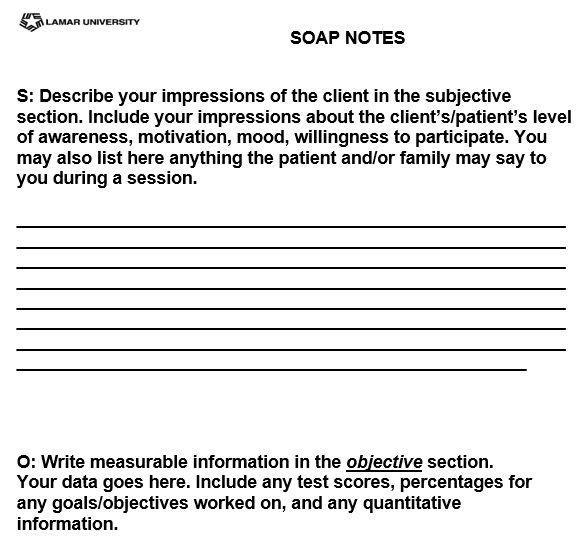
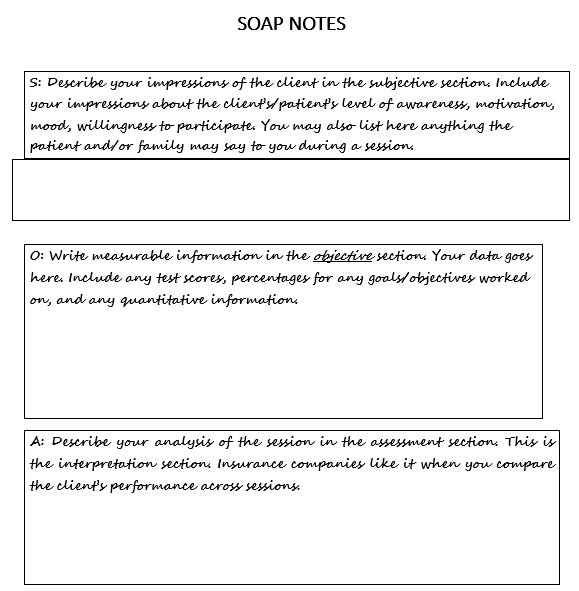
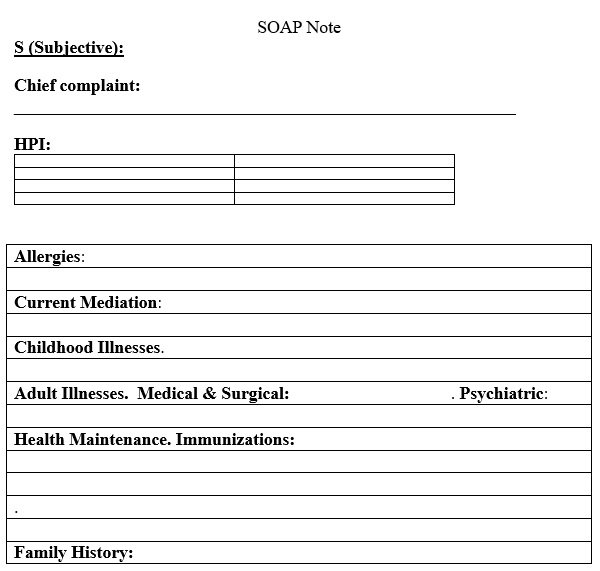
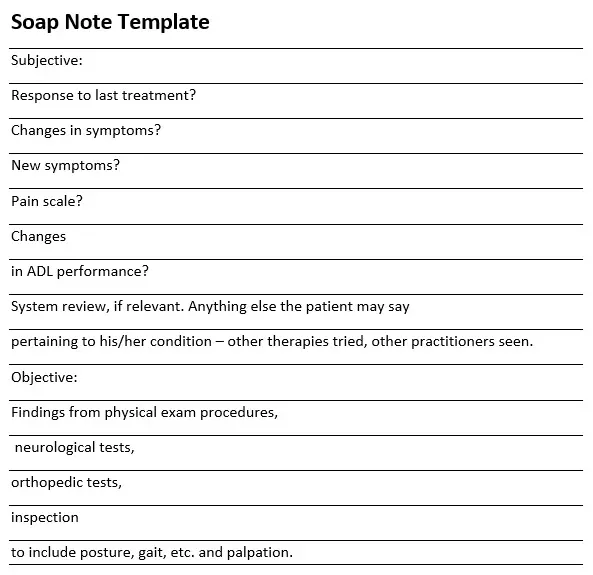
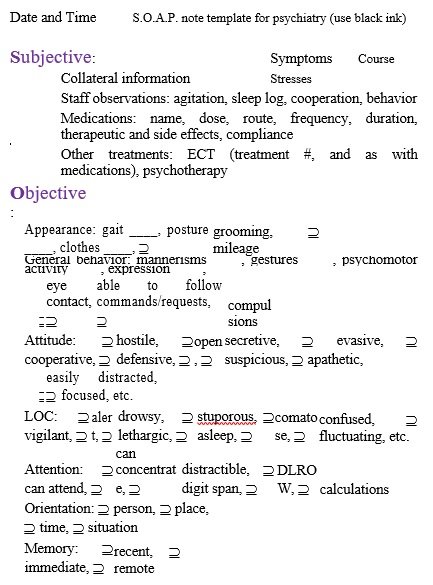
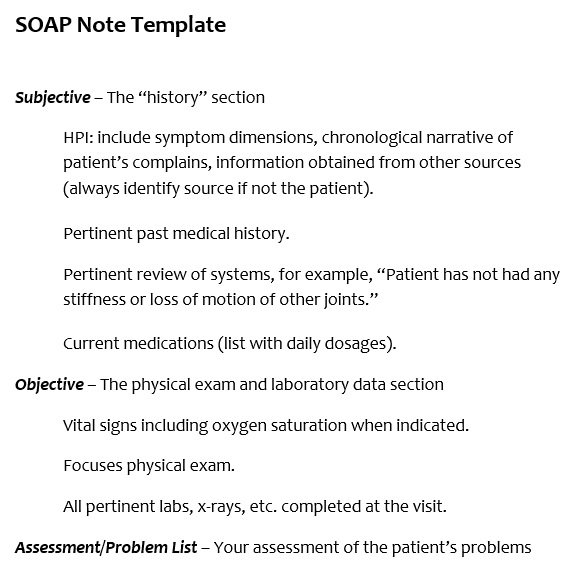
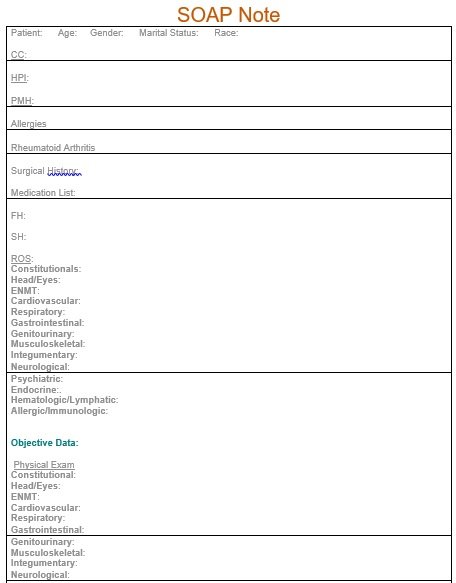
Subjective:
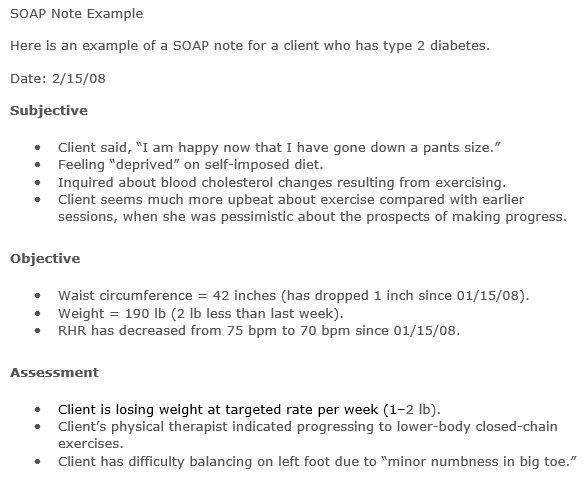
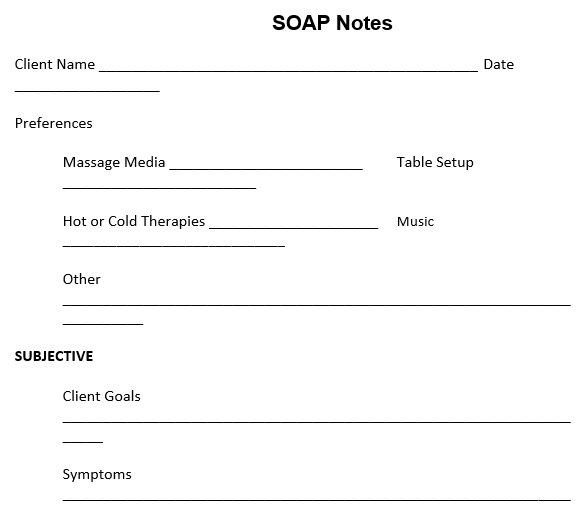
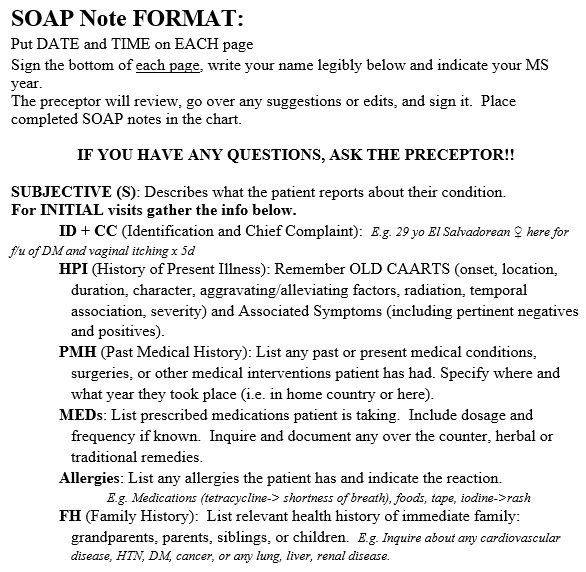
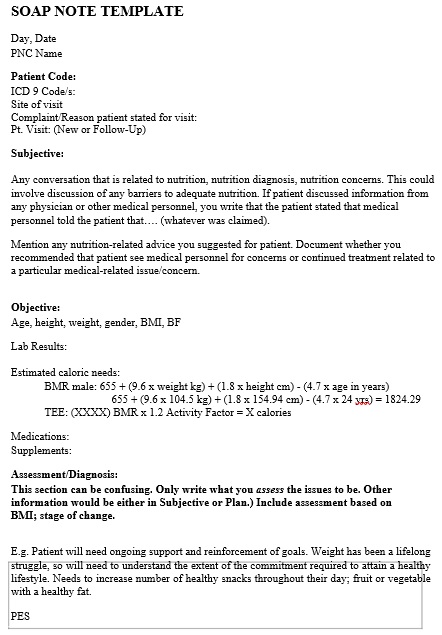
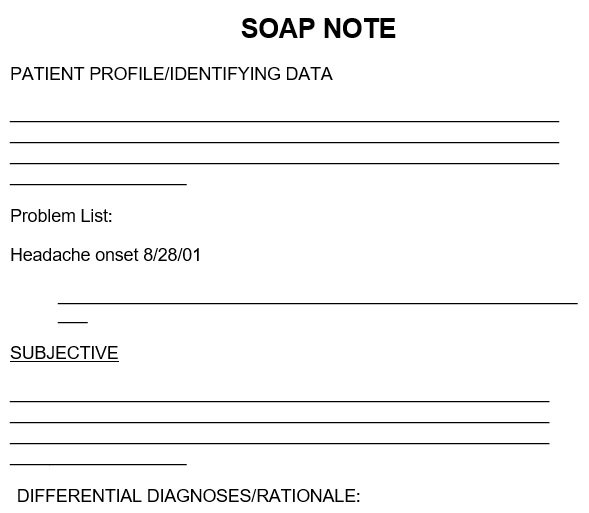
The subjective component is written in a narrative form. It describes the recent condition of the patient. Patient’s complaints are also recorded in this section and could be worded using the patient’s own words. This document mainly focuses on the following reasons;
- It contains the reason for the injury or illness. Mention the exact date that when the symptoms have started.
- A chronology of symptoms of the illness i.e. when the patient first began to experience symptoms, when it got worse, and when the patient had gone to the hospital.
- State the body parts that are affected or the specific area of the body that is in pain.
- It also includes a detailed description of the illness and the quality and severity of the symptoms. Indicates the factors which have affected the patient.
- Discuss the treatment which was given to the patient before the hospital visit.
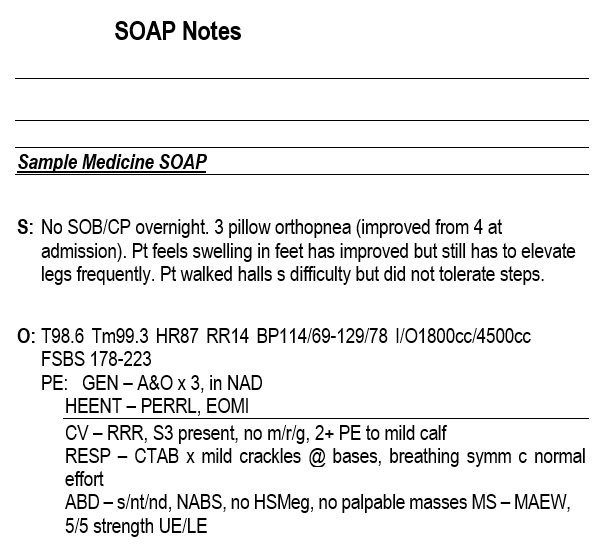
Objective:
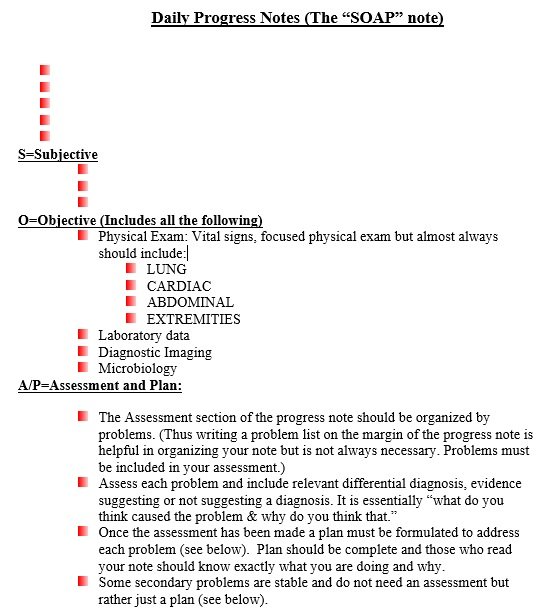
The objective component is a factual account of the patient and the patient’s status. It contains the following information;
- It contains the physical measurements of the patient like height, weight, etc.
- The patient’s posture, any wounds or bruising, visible injuries, high temperature, or any other abnormalities are included in this component.
- Results of laboratory examinations such as urine, stool, blood, etc.
- The patient’s reactions during treatment such as nervousness, flinching, grimacing, or any other indicators may signal a deeper issue.
- Objective statements, findings, and observations are related to the subjective component.
Assessment:
On the basis of the first two components, this component contains the initial diagnosis of the physician. However, along with the diagnosis of the illness or injury, the assessment must contain all the symptoms stated by the patient. Arrange a differential diagnosis in order of the most likely one to the least likely one. All possible cause of the patient’s problem is also discussed in it.
Furthermore, emphasize the progress of the patient’s health that had been made since the last visit along with overall progress towards fully treating the symptoms. Include any drug-related issues as well as evidence and reason behind it. In order to make a detailed and comprehensive assessment, discuss all the risk factors.
Plan:
The final component, plan, states the procedure that the physician will be doing to treat the patient. To treat a patient, the physician can refer to specialists, and important procedures can be performed. Additionally, if therapy is recommended then specify the goals of the therapy along with any drugs. Also, if the patient has more than one problem, mention each and every item in the differential diagnosis.
Both assessments and plan components are commonly grouped together to make things a lot easier. These are the important components in all soap notes. They are effective and must be added to the medical record of the patient.
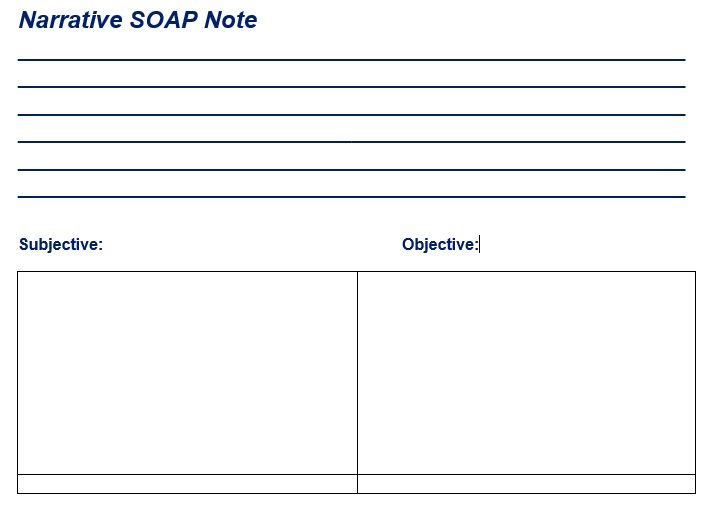
How to write SOAP Note Template?
Here are some steps and tips to write effective soap notes;
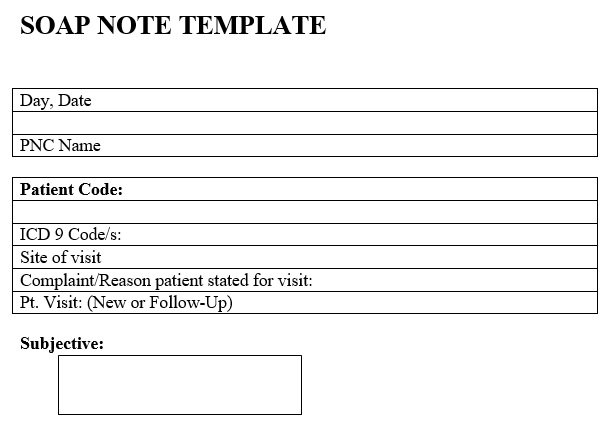
- At first, download the editable and printable soap note template from any website. Then, provide all the information in the subjective portion. You can get this information from the patient.
- To make a great narrative for the subjective component of the note, ask questions from the patient in order. The most important information is the patient’s history of injuries or illnesses.
- Don’t ask questions that lead to yes or no answers. In this way, you would not get the needed information.
- After that, go to the objective component and write what you as a physician have observed from the patient.
- During questioning, you are examining and observing the patient’s behavior.
- By evaluating the symptoms, write down the injuries and probable illnesses. Next, check the results of the examinations you have made.
- On the basis of objective reports, record all the assessments you have made. You should arrange the list of diagnoses according to possible likelihood.
- You should narrow down the plan of action that you give to the patient. Discuss all the therapies, drugs, and treatments in detail.
- You should use it as a reference for daily procedures so make it in detail.
Some tips for effective SOAP notes and assessments:
Here are some tips for you;
- You should always use SOAP note template in order to make the documentation of healthcare assessment standardized.
- For SOAP note documentation, you must follow your facility’s procedures and policies. This will make sure uniformity and compliance.
- The SOAP note process is used by all healthcare team members to document their findings. This way, you have a complete patient record and it will also ease the workflow for all facility staff.
- When completing the SOAP note template, you must use eligible handwriting in order to improve the accuracy and legibility of the document.
- Before filling or transmitting SOAP notes to another healthcare professional, you should thoroughly review them. Keep in mind that the main aim of these notes is to give a full report of patient assessment.
- You should submit SOAP notes when you completely assure that they contain all pertinent information and don’t miss any important information.
- Make sure that your SOAP note is formatted accurately and easy to read.
- When filling out SOAP note templates, healthcare professionals should use an erasable pen so that they can correct any mistakes easily.
What are the benefits of using the SOAP note template?
Here are the benefits of using the SOAP note template;
Consistency
Your progress notes will have a consistent format if you use a SOAP note template. Make use of consistent templates to simplify your writing process. Also, it will make it easier for other providers to read your notes.
Accuracy
Along with making things easier for you, the SOAP note template improves the quality of your documentation. To cover all the right information, you should make four different sections in your notes.
Save time
You can save a lot of time by using the SOAP note template as your documentation is already formatted well and you just have to fill in the information.
Difference between the SOAP note and a simple note:
The SOAP note is a medical note used by the healthcare professionals. They use it to accurately document and record patient’s condition during treatment.
On the other hand, a simple note is used by anyone to write down important information that they don’t want to forget.
Conclusion:
In conclusion, a soap note template is used by doctors, nurses, and other health professionals in charge of treating patients. Writing notes is beneficial in order to keep a record of the progress of treatments of patients. These notes are added to the records of patients. It acts as evidence that there had been regular patient contact throughout the whole treatment period.